Jan 31, 2019
Scientists Rethink Psychedelics As Attitudes Change Toward Formerly Illicit Drugs
Robin Seaton Jefferson
Contributor
The irony. The generation who brought psychedelic drugs to the attention of the world, may just be the ones who use them as medicine to treat anxiety and depression or simply to face death.
But while researchers around the world are looking at some formerly illicit drugs in a new way, they’re doing it with caution. They still contend that while initial findings may be encouraging, research is at an early stage and patients should never attempt to self-medicate.
Mind Fog series. 3D rendering of human face morphed with fractal paint suitable as a backdrop for the projects on inner world, dreams, emotions, creativity, imagination and human mind GETTY
Researchers at Johns Hopkins University recently suggested that the FDA’s classification for psilocybin— the psychoactive compound that occurs naturally in hallucinogenic or magic mushrooms—be changed from a Schedule I drug, which has no known medical benefit, to a Schedule IV drug, which is similar to conventional prescription drugs.
The
analysis, published in Neuropharmacology in October, was part of a review assessing the safety and abuse of medically administered psilocybin under the
US Controlled Substances Act (CSA). But it also potentially paves the way for the psychedelic drug to perhaps some day treat depression and anxiety and possibly even alcohol abuse and to help people stop smoking.
In America as well as other countries around the world, people have been rethinking their attitudes about formerly illegal substances, and their potential use for all sorts of mental and physical maladies. And scientists are no exception. The widespread legalization of marijuana across America has helped to demystify drug use and cause many to question why it was illegal in the first place.
Psychedelics, like Lysergic Acid Diethylamide LSD, psilocybin and mushrooms, are currently illegal and not approved for medical or recreational use. And researchers caution that before the FDA can be petitioned to reclassify the drug, extensive study and trials—which can take more than five years—would have to be conducted.
And overeall, while they admit more studies are needed, Johns Hopkins researchers concluded that "psilocybin can provide therapeutic benefits that may support the development of an approvable New Drug Application (NDA)."
Here's why:
Psilocybin mushrooms have been used for millennia for spiritual and medical purposes.
Animal and human studies indicate low abuse and no physical dependence potential.
Major national surveys indicate low rates of abuse, treatment-seeking and harm.
Psilocybin may provide therapeutic benefits supporting its development as a new drug.
Analysis supports the scheduling of psilocybin no more restrictively than Schedule IV.
Study authors reported that "Research suggests the potential safety and efficacy of psilocybin in treating cancer-related psychiatric distress and substance use disorders, setting the occasion for this review.
A more extensive assessment of abuse potential according to an 8-factor analysis would eventually be required to guide appropriate schedule placement."
While researchers list potential harms of the drug as: dangerous behavior in unprepared, unsupervised users, and exacerbation of mental illness in those with or predisposed to psychotic disorders, they nonetheless admit that the “scope of use and associated harms are low compared to prototypical abused drugs, and the medical model addresses these concerns with dose control, patient screening, preparation and follow-up and session supervision in a medical facility.”
Authors of the Johns Hopkins research concluded that:
Psilocybin has an abuse potential appropriate for CSA scheduling if approved as medicine.
Psilocybin can provide therapeutic benefits that may support the development of an approvable
New Drug Application (NDA) but further studies are required.
The adverse effects of medical psilocybin are manageable when administered according to risk management approaches.
Although further study is required, placement in Schedule IV may be appropriate if a psilocybin-containing medicine is approved.
According to a New York Times
article by Laura M. Holson, “
Microdosing, or the use of psychedelics in small, managed doses, has become a popular way to try to increase productivity and creative thinking, particularly among the technorati in Silicon Valley. It’s even a plot point in the CBS show ‘The Good Fight.’”
Holson goes on to write, though, that for decades researchers have shunned the study of psychedelics and that “research stopped, in part, because the use of mind-altering drugs like LSD and mushrooms became a hallmark of hippie counterculture.”
The new study, which reviewed data going back to the 1940s, was undertaken by Dr. Matthew W. Johnson, an associate professor of psychiatry and behavioral sciences at Johns Hopkins School of Medicine; Roland R. Griffiths, a professor in the departments of Psychiatry and Behavioral Sciences, and Neuroscience at the Johns Hopkins University School of Medicine.
Johnson told the New York Times the data suggests that psychedelics are powerful behavioral agents, and if psilocybin were to be approved for patients, “I see this as a new era in medicine.” Still, researchers called for strict controls on the drug’s use, especially for patients with psychotic disorders and anyone who takes high doses of the drug.
Research continues around the world with scientists trying to find positive ways to use drugs that have for decades been demonized. And a number of clinical trials have been conducted over the past decade that are yielding promising results regarding the safety and effectiveness of psychedelics in patients with conditions such as depression and addictions.
Patients in a 2017 Imperial College London
study taking psilocybin to treat depression show reduced symptoms weeks after treatment following a 'reset' of their brain activity.
In the first
study with psilocybin in depression, researchers used psilocybin to treat 20 patients with treatment-resistant depression.
The individuals were given two doses of psilocybin (10 mg and 25 mg), with the second dose a week after the first.
In their
paper published in Scientific Reports, researchers described patient-reported benefits lasting up to five weeks after treatment.
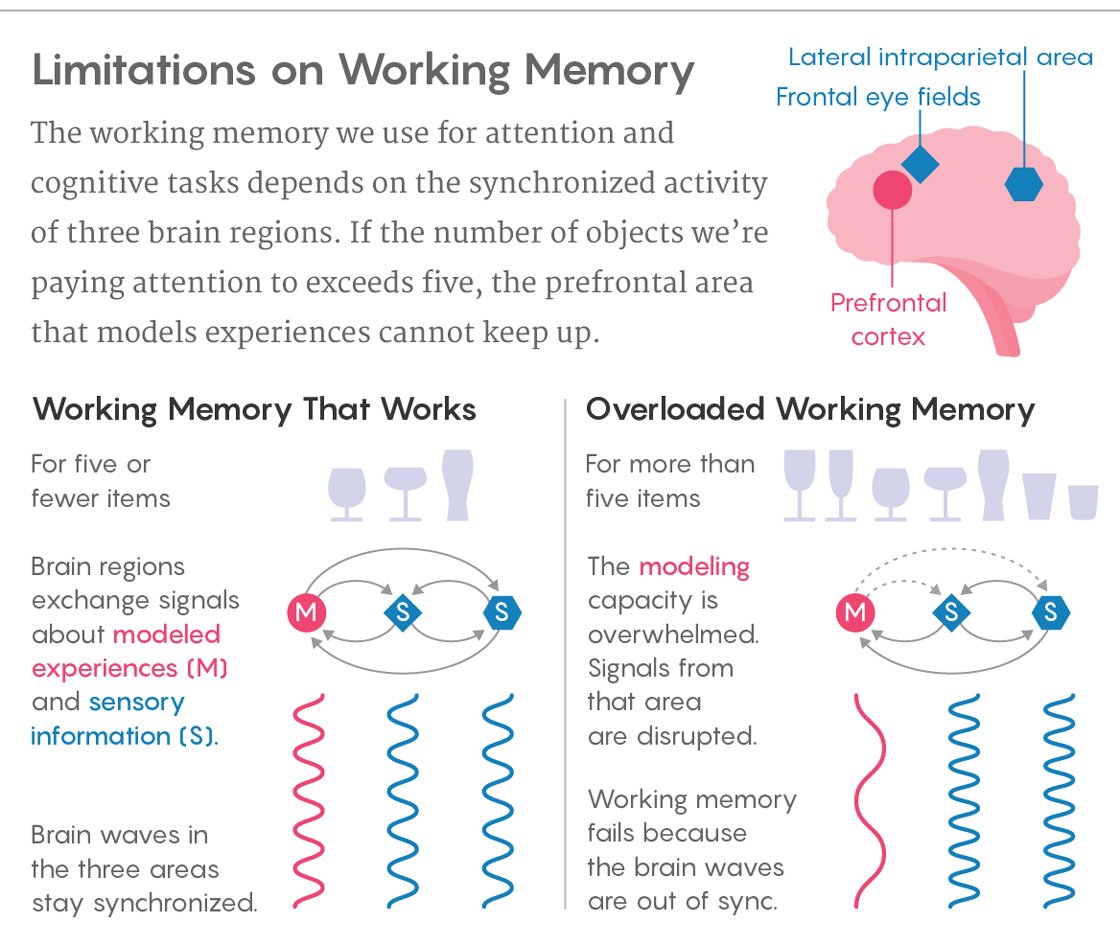
Researchers said that while the sample size was limited and there was no control group, they nevertheless believe the psychedelic compound “may effectively reset the activity of key brain circuits known to play a role in depression.”
Robin L Carhart-Harris, head of the Psychedelic Research Group (PRG), Psychopharmacology Unit, Centre for Psychiatry and Department of Medicine at the Imperial College London, compared images of patients’ brains before and one day after they received the drug treatment.
Researchers said those images revealed changes in brain activity that “were associated with marked and lasting reductions in depressive symptoms.”
In another
study, researchers from Imperial College London, working with the
Beckley Foundation, for the first time visualized the effects of LSD on the brain.
Research from the same group, part of the Beckley/Imperial Research Programme, in a study published in the journal
European Neuropsychopharmacology, revealed that listening to music while taking LSD triggered interesting changes in brain signaling that were associated with eyes-closed visions.
In that study, researchers found that the combination of LSD and music caused this region to receive more information from an area of the brain called the parahippocampus—the region involved in mental imagery and personal memory, and “the more it communicated with the visual cortex, the more people reported experiencing complex visions, such as seeing scenes from their lives.”
Speaking on the 2017 study of psilocybin, Carhart-Harris said,
“We have shown for the first time clear changes in brain activity in depressed people treated with psilocybin after failing to respond to conventional treatments.
Several of our patients described feeling ‘reset’ after the treatment and often used computer analogies.
For example, one said he felt like his brain had been ‘defragged’ like a computer hard drive, and another said he felt ‘rebooted.’
Psilocybin may be giving these individuals the temporary ‘kick start’ they need to break out of their depressive states and these imaging results do tentatively support a ‘reset’ analogy.
Similar brain effects to these have been seen with electroconvulsive therapy.”
Carhart-Harris said in his study, functional MRI imaging revealed reduced blood flow in areas of the brain, including the amygdala, a small, almond-shaped region of the brain known to be involved in processing emotional responses, stress and fear.
“Psilocybin may be giving these individuals the temporary ‘kick start’ they need to break out of their depressive states,” Carhart-Harris said.
"Based on what we know from various brain imaging studies with psychedelics, as well as taking heed of what people say about their experiences, it may be that psychedelics do indeed ‘reset’ the brain networks associated with depression, effectively enabling them to be lifted from the depressed state."
Analysis of the data from these same patients has hinted that the psychedelic substance could also lead to lasting changes in outlooks, including how people feel about the natural environment and even their political views.
According to the researchers, patients report feeling more connected to nature months after treatment, as well as a general shift along an axis of authoritarian and libertarian viewpoints.
Study authors warn that “while the initial findings are encouraging, the research is at an early stage and that patients with depression should not attempt to self-medicate, as the team provided a special therapeutic context for the drug experience and things may go awry if the extensive psychological component of the treatment is neglected.”
The PRG at Imperial focuses on two main research areas:
1) the action of psychedelic drugs in the brain, and
2) their clinical utility, e.g. as aides to psychotherapy, with a particular focus on depression.
Researchers at the PRG were unavailable for comment on the study.
“The PRG is currently gearing up for a clinical trial, so their attention is fully focused on the research for the time being,” a spokesperson for Imperial College London said in response to inquiries about where the new research stands.
The Medicine Research Officer said researchers are currently working on more robust designs including testing psilocybin against a leading antidepressant in a clinical trial.
In still another study at PRG, researchers attempted to distinguish between the near-death experience and the psychedelic trip. Published last year in the journal Frontiers in Psychology their
findings indicate that DMT may produce similar effects in the brain.
According to the researchers, DMT is a potent psychedelic found in certain plants and animals, and is the major psychoactive compound in ayahuasca, the psychedelic brew prepared from vines and leaves and used in ceremonies in south and central America.
“Near-death experiences, or NDEs, are significant psychological events that occur close to actual or perceived impending death," Imperial College reported.
"Commonly reported aspects of NDEs include out of body experiences, feelings of transitioning to another world and of inner peace, many of which are also reported by users taking DMT.”
Carhart-Harris said DMT is “a remarkable tool that can enable us to study and thus better understand the psychology and biology of dying.”
The Imperial College London team looked at 13 healthy volunteers over two sessions.
They gave participants intravenous DMT and placebo, receiving one of four doses of the compound.
The PRG researchers compared the participants’ experiences against people who had previously reported actual NDEs and who had completed a standardized questionnaire to try and quantify their experiences.
The group were asked a total of 16 questions including ‘Did scenes from your past come back to you?’ and ‘Did you see, or feel surrounded by, a brilliant light?’
“The team found that all volunteers scored above a given threshold for determining an NDE, showing that DMT could indeed mimic actual near death experiences and to a comparable intensity as those who have actually had an NDE,” researchers reported.
Carhart-Harris said the "DMT is a remarkable tool that can enable us to study and thus better understand the psychology and biology of dying.”
Professor David Nutt, Edmond J Safra Chair in Neuropsychopharmacology at Imperial, said: “These data suggest that the well-recognized life-changing effects of both DMT and NDE might have the same neuroscientific basis.”
Still researchers admit there are subtle, but important differences between DMT and NDE responses.
The “DMT was more likely to be associated with feelings of ‘entering an unearthly realm,’ whereas actual NDEs brought stronger feelings of ‘coming to a point of no return.’
The team explain that this may be down to context, with volunteers being screened, undergoing psychological preparation beforehand and being monitored through in a ‘safe’ environment.”
Some research is even going back in history to study what many feel was research left unfinished.
A recently published
thesis, written by Michael James Christopher Lyons at the University of Saskatchewan, explores one therapeutic model for problem drinking which was developed in Saskatchewan in the mid-twentieth century.
The therapy, which drew on the psychedelic properties of LSD and the program structure of Alcoholics Anonymous (AA), “not only showed a high rate of success but also served as a mechanism for spiritual growth and development for some patients,” Lyons wrote.
In his thesis, Lyons presents the perspectives of both the psychiatric professionals and Christian clergy who were involved in these trials as well as the perspective of a patient who underwent the therapy to examine how LSD and AA were used to treat problem drinking and how it blurred the lines between science and religion.
“On a December day in 1960, Baptist minister Reverend William Potoroka had one of the most transcendent spiritual experiences of his life.
It was an event that would reframe his understanding of science, spirituality and of his own personal vocation,”
reports PRØHBTD, who describes itself as the premier online lifestyle destination for modern cannabis enthusiasts.
“I felt that I was ascending a spiral staircase and that this was leading me up, up, into the light,’” he recalled. ‘It was as if my ascent would soon put me within gazing distance of God and his throne.’'
Potoroka’s encounter occurred at the Weyburn Mental Hospital in Saskatchewan, Canada.
The reverend went to the hospital to investigate an experimental treatment for alcoholism—LSAD.
In the study, 10 male patients who suffered from alcoholism received psychiatric treatments, like patient interviews and group therapy, while also attending weekly meetings at the local AA chapter in Weyburn.
By the eighth week, if patients had still not improved, they were given LSD.
“As Lyons points out in his thesis, prior to being considered illegal drugs, psychedelics—and particularly LSD—were being studied by medical establishments around the world with the intention of using them to treat various psychiatric disorders,” PRØHBTD reported. “From 1950 to 1965, close to 40,000 patients were given LSD for conditions ranging from schizophrenia to post-traumatic stress disorder (PTSD).
Many early results appeared promising, with a series of positive reports on the drug’s benefits appearing in Time magazine and high-profile figures such as actor Cary Grant publicly lauding how LSD helped him succeed in conquering mental issues where standard talk therapy, hypnosis and yoga had all failed.
In 1956, the American Medical Association (AMA) officially declared alcoholism a disease.
This distinction led the psychiatric community to seek out biochemical solutions for a problem that had previously been thought of as a moral failing.
As LSD was then being explored as a potent yet little-understood cure for a slew of psychological issues, clinical trials to treat alcoholism with LSD were soon underway.
The goal of the earliest of these trials was to use LSD to mimic the temporary psychosis caused by alcohol withdrawal known as delirium tremens, thereby scaring the patient away from alcohol consumption via a sort of aversion therapy.
But this method didn’t work very well, considering, as Lyons explains, that instead of reacting to their experience with horror, ‘patients often responded favourably [sic], claiming to enjoy the experience, and even suggested that it had provided a window into a spiritual environment/landscape.’
Realizing that perhaps the self-reflective insights that their patients reported might be a more effective avenue toward recovery than chemically induced terror, doctors at the University of Saskatchewan and the Weyburn Mental Hospital—Abram Hoffer, Humphry Osmond and Sven Jensen—decided to change their approach.
Instead of attempting to stimulate delirium tremens, they began a series of trials that would pair LSD's novel capacity for prompting self-examination and spirituality with a far less invasive treatment for alcoholism—Alcoholics Anonymous (AA).”
Though Potoroka found himself at the intersection of the age-old debate between science and religion, he described his healing experience with LSD this way: "Through a several-staged experience of being pulled upward, or of aspiration, I believe that I received an enhancement of my idea of God and grace.
This came to me from what I believed before the experience and how much more God and grace mean to me because of the experience. LSD helped me so to make contact with the spiritual treasures I knew of… [and] I found new riches there."
When reporting on his experience with LSD to the church, Potoroka wrote, “Alcoholism was regarded as an illness of the body, the mind and the spirit.
The LSD treatment is a way of getting at two of the three sides of the illness—the mind, and especially the spirit.”
So whether Potoroka has reconciled the divide between the medical and spiritual communities, Lyons acknowledged that “the field of psychedelic research occupied the intellectual space of both mysticism and biomedical practices.”

















 Henri Cartier-Bresson
thanks to
Henri Cartier-Bresson
thanks to